Families struggling as health bodies in India change guidelines for COVID | Coronavirus News Plague

New Delhi, India – Late last month, the Indian government radically changed its approach to hospital care for COVID-19, which led to chaos and confusion when people realized that the drugs had been reduced.
For several months, I had read and rewritten my family notes, remembering what I could give, and going to the local hospitals for immediate delivery. Like thousands of others, I had read hundreds of petitions on these issues.
What if the government leaves them? As I went through the research, I also recalled that ivermectin, one of the drugs that has now been downloaded and evaluated in depth, was given to me by a dermatologist in July last year.
“Only one pill, tonight,” said the doctor. I was told that it was an antiseptic, used to remove worms and scabies.
But little did I know that two months later, I would be given ivermectin as part of my COVID treatment.
During a telephone interview, the doctor prescribed 5 days of doxycycline (anti-bacterial drug) and one day of ivermectin.
Later that day, when the state health workers came to our house, my husband, who was suffering from COVID-19, was given a packet of hydroxychloroquine and told to take the pills for seven days.
We all jumped.
The drugs, which were popular at the time, became increasingly important as former US President Donald Trump threatened to cut off drugs if India reduced its exports to the United States.
This was the first wave. Although there were many difficulties for migrants in India on their way home, people are losing their lives and the economic downturn that has resulted from unemployment, high mortality rates, and hospitals and air is not in short supply.
The second river, which we all think many accounts could be weak, was about to destroy us.
In April, a second tidal wave hit our home. My whole family – my husband, my mother and my in-laws – received COVID-19, some even vaccinated. We were trapped inside a dangerous epidemic while hospital beds, air and medicine were missing.
My mother-in-law with COVID was given ivermectin for about a week. He was also given an ani-virus, favipiravir, also known as fabiflu.
By the time he was hospitalized on May 2 for pneumonia, he had already been given ivermectin, doxycycline, azithromycin and favipiravir. In the hospital, they also give remdesivir and plasma drugs – twice.
We also used cell phones to put him in the hospital with a ventilator. We did the same for my mother when she was received on May 11.
The only difference: by the time they arrived at the hospital for pneumonia, the bloodstream had been dropped from the coronavirus protocol.
But here it was on April 2021. The Indian Council of Medical Research (ICMR), the country’s highest scientific body, had declared a “bloodless medicine” earlier in November 2020.
In a press release on November 17, 2020, ICMR stated that “PLACID, the world’s largest plasma test, did not show the benefit of CPT in patients”.
On June 10 this year, Samiran Panda, head of ICMR’s epidemiology and infectious diseases, confirmed to me that plasma treatment was said to have not benefited from ICMR.
On other drugs such as ivermectin, he said all the evidence came from observational studies, which showed that it could be useful but “no clinical trials are monitored in two ways”.
“There is no longer sufficient evidence for the use of doxycycline, favipiravir and hydroxychloroquine,” he said.
Most of these drugs were part of the COVID-19 medical guidelines until May 27. But they were not approved by the World Health Organization or the Food and Drug Administration (FDA) of the US.
However, many doctors believe that plasma products may have saved lives.
Dr Manoj Luthra, director of the cardiac surgery department at Jaypee Hospital in Noida, a city outside New Delhi, told me that “although plasma drugs may be phased out by the government, there is ample evidence available by doctors regarding its effectiveness as a treatment option. COVID-19 “.
“Some of us have also sent to the government about this,” he said, sharing an article entitled Emerging Evidence Exercise the Efficacy of Ivermectin in Prophylaxis and Treatment of COVID-19, published in the American Journal of Therapeutics.
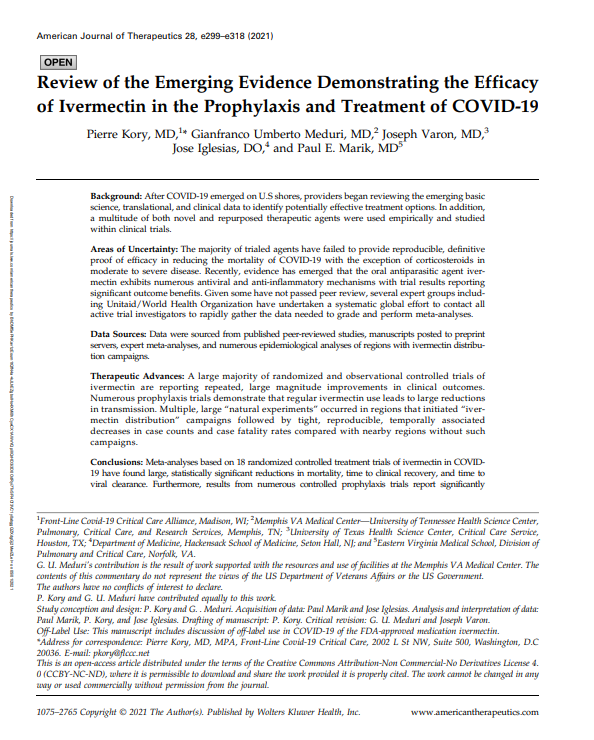 An American Journal of Therapeutics article shared by Dr. Manoj Luthra [Al Jazeera]
An American Journal of Therapeutics article shared by Dr. Manoj Luthra [Al Jazeera]
But by April, concerns had spread to other drugs, such as the overuse of steroids in the treatment of coronavirus. My mother and mother-in-law were all given steroids for the past month.
In May, we learned that new government guidelines may instruct hospitals to use steroids for no more than 10 days or until the time they are prescribed, according to a previous report.
Steroids, which have been useful in reducing lung inflammation in COVID-19 patients, are considered to be life-saving when given to patients at the right time and at the right time. But it also lowers immunity and raises blood sugar.
Bishnu Panigrahi, chief medical officer at Fortis, one of India’s largest medical groups, said “according to steroids, they have been misused”.
He said steroids were used “too early during treatment, in high doses and over time, which causes secondary infections”.
“Black fungus is a problem for misuse of steroids,” he said.
Black mushroom, or mucormycosis, is a rare but serious disease that kills 50%. It affects the sinuses, brain and lungs and can kill patients with immunodeficiency.
In India, the disease has increased by 1.5 percent, with 31,216 cases and 2,109 deaths during the second wave so far.
Black mushroom is now listed as a pandemic under the Epidemic Diseases Act by the Indian government.
As concerns mounted due to drug abuse, the government radically changed its approach to health care by the end of last month.
On May 27, the Directorate General of Health Services (DGHS), under the auspices of the Ministry of Health, discontinued all prescription drugs, including ivermectin, azithromycin, doxycycline, zinc, favipiravir and plasma drugs.
DGHS has only been recommended for antipyretics (drugs used to prevent or reduce malaria) and antitussives (to relieve or suppress coughs) in mild patients, and there is no prescriptive drug or study for patients without it.
Steroids and anticoagulants have been prescribed in less severe cases, and oxygen therapy, intubation, ventilation and modulators are assisted in severe cases.
The medical body also stored remdesivir (for severe to severe cases) and tocilizumab, an immunosuppressant prescribed by those who are very sick.
The new DGHS guidelines have been widely accepted, including WHO, which Chief Scientist Soumya Swaminathan wrote: “Evidence-based advice from @mohfw DGHS – simple, clear and concise advice for physicians.”
Swaminathan said the guidelines “can be revised as soon as new evidence becomes available”.
However, the guidelines provided by the Ministry of Health and ICMR continue to recommend ivermectin and hydroxychloroquine in rare cases. It was not changed or modified until the report was published.
So far, COVID-19 guidelines have been provided by DGHS, the federal health ministry, ICMR and government agencies. And they are not always the same.
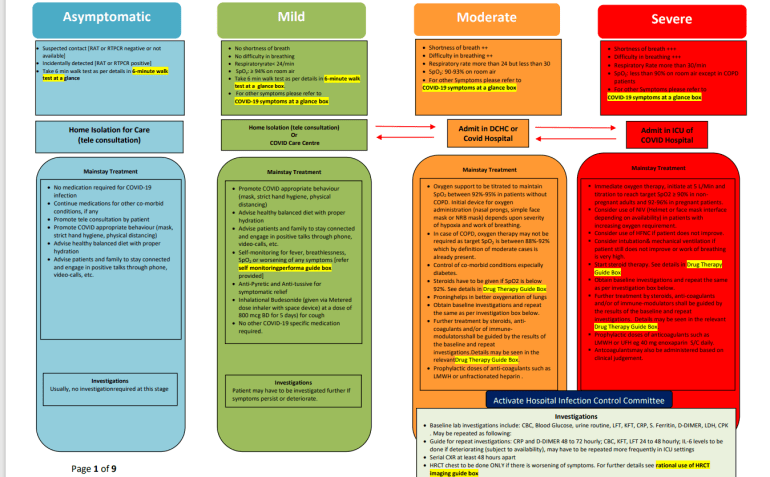 COVID guidance provided by the Directorate General of Health Services in India (DGHS) in India [Al Jazeera]
COVID guidance provided by the Directorate General of Health Services in India (DGHS) in India [Al Jazeera]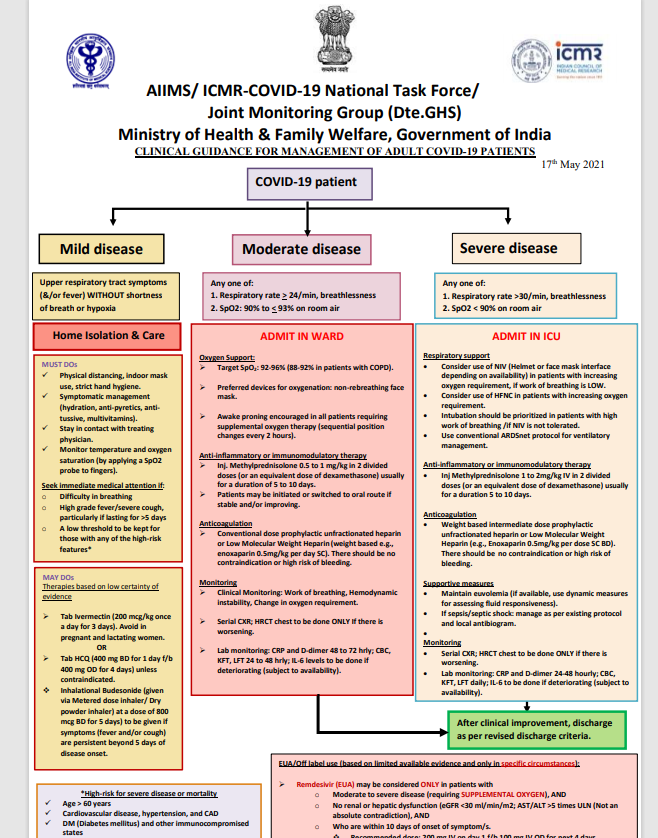 Advice from the Indian Council of Medical Science (ICMR) [Al Jazeera]
Advice from the Indian Council of Medical Science (ICMR) [Al Jazeera]
As a result, although almost all currently used anti-COVID-19 drugs have been discontinued, remdesivir, a drug used for the treatment of Hepatitis C, has been retained by DGHS in its health regimen. The drug is approved by the FDA and is used in several other countries to treat coronavirus infection.
But like everything else, there is no big deal though.
Panigrahi of Fortis Hospitals says there has been “a widespread use of remdesivir, which is due to the high pharma that is aggressively enforcing the drug, although the literature does not show a decrease in mortality”.
However, DS Rana, medical superintendent at Sir Ganga Ram Hospital in New Delhi, one of the largest facilities at COVID headquarters, is said to be an effective anti-viral drug.
“Well-conducted trials have shown that if the drug is used early in the viral phase, it can have a positive effect on faster recovery from COVID in the case of hospitalization. DGHS has recommended the proper use,” he said.
 ICU at Sir Ganga Ram Hospital in New Delhi [Courtesy of Sir Ganga Ram Hospital]
ICU at Sir Ganga Ram Hospital in New Delhi [Courtesy of Sir Ganga Ram Hospital]
While there is no one-size-fits-all approach right now, and trial and error are part of the fight against undiagnosed viruses, evidence should be reviewed regularly to change treatment options to minimize the risk of clinical trials.
According to government approval, the third virus is “inevitable”.
Experts say that examples and examples available in the US and Europe show that vaccination of at least 30 to 40% of people by the end of the year could be a way to prevent the virus.
So far, less than 5 out of 950 million Indians have been fully vaccinated.
The total number of COVID-19 cases so far is about 30 million, with 381,903 people dying as of Thursday. About 200,000 people died during the second COVID.
As a result, anxiety is growing as a result of relapse, recurrence of the virus and other diseases even though the disease has fallen sharply in the last two weeks.
The Indians hope that the new government’s vaccination guidelines, announced on June 7, will help make this possible.
Under the new regulations, effective June 21, the government will provide 75% of the vaccine and provide it free of charge. The remaining 25% shots will be available in public hospitals.
While global trends show that the prevalence of morbidity and mortality is declining with increasing vaccination, the Indian government needs to improve its COVID-19 treatment regimens and adapt it to global developments.
As for my family, my mother still has the virus and my mother-in-law continues to suffer from COVID.



